Breast cancer is a common malignant tumor disease. According to medical statistics, it is diagnosed in about 10% of females, while the highest prevalence of pathology is observed in Europe. Most cases of morbidity occur over the age of forty-five years. It should be noted that in developed countries there is a tendency to reduce the incidence rate due to early screening of the disease.
As a rule, malignant neoplasms of the breast have a heterogeneous structure and consist of different types cells with different growth rate and response to therapy. Therefore, it is not always possible to accurately predict exactly how the pathology will develop. In some cases, tumor growth occurs very slowly and is practically asymptomatic for a long time; in other situations, deterioration occurs rapidly. The success of breast cancer treatment depends on good early diagnosis.
Reasons for the development of breast cancer
It is possible to identify a large number of factors that in one way or another can contribute to the occurrence of breast cancer. The underlying causes of the development of a dangerous disease are associated with genetic or hormonal changes. In the latter case, an increase in estrogen activity has an effect on the formation of a malignant tumor.
To the risk factors of malignant processes mammary gland include:
Attention . Numerous studies show that the risk of developing breast cancer increases in women of high stature, as well as overweight women in the postmenopausal period.
All of the above factors do not cause cancer directly, but create a favorable background for the development of malignant processes. Certainly, excess weight and high growth does not yet mean that a woman will definitely have cancer, but such circumstances can increase the risk of its occurrence. As a rule, the formation of a tumor occurs under the influence of several provoking factors at the same time.
Breast cancer: varieties and signs
In clinical practice, there are several types of malignant breast tumors:
Like most malignant diseases, breast cancer is very difficult to detect in the early stages, as it may not have clinical manifestations for a long time. Severe soreness, swelling, discomfort, retraction of the nipples, pathological discharge from them, and any other symptoms require an urgent referral to a specialist.
Note!If you feel some kind of seal in the chest, even in the absence of other symptoms, it is better to immediately consult a doctor to find out the nature of the neoplasm.
To determine the degree of the disease, a special table is used: the letter T indicates the state of the primary tumor, M - the presence of metastases in other organs, N - the tumor has metastasized to regional lymph nodes.
A malignant neoplasm can be localized in various parts of the mammary gland: in the area of the skin, areola and nipple, in the area of \u200b\u200bthe upper or lower inner square of the gland, the upper or lower outer square, in the posterior axillary part, etc.
Early diagnosis of breast cancer
 Early diagnosis of neoplastic diseases of the mammary glands should include regular self-examination, a visit to a mammologist. After the age of forty, it is recommended to undergo a mammography procedure annually for preventive purposes.
Early diagnosis of neoplastic diseases of the mammary glands should include regular self-examination, a visit to a mammologist. After the age of forty, it is recommended to undergo a mammography procedure annually for preventive purposes.
It is advisable to do a self-examination of the breast every month on the fifth to seventh day of the menstrual cycle. When examining, special attention should be paid to the symmetry mammary glands, the condition of the skin and nipples, as well as whether the size of one breast has changed. Palpation can be performed in the supine or standing position. In turn, it is necessary to feel both glands with your fingertips, starting from the nipple towards the outer part. Alarm signals will be any seals in the tissues of the breast or in the nipple. You should also pay attention to the condition of the lymph nodes in the subclavian and axillary region.
If you find suspicious symptoms, you should contact a specialist.
An accurate diagnosis can only be made after a comprehensive examination, including the following diagnostic methods:
- examination by a mammologist;
- mammography;
- ductography;
- ultrasound procedure;
- biopsy of neoplasm tissue;
- laboratory studies of discharge from the nipple;
- blood test for hormones and tumor markers.
Important! For the purpose of early diagnosis of breast cancer, all women who have crossed the forty-year milestone are recommended to undergo three screening studies annually: mammography, hormonal blood test and a study for CA 15-3 tumor markers.
With the diagnosis of breast cancer, the degree of spread of a malignant tumor is determined by the results of additional diagnostic methods:
- chest x-ray,
- bone research,
- ultrasound abdominal cavity and others.
Methods of treatment of breast cancer
 Modern methods of breast cancer treatment include surgery, chemotherapy and radiation therapy, as well as hormonal and immunotherapy. Therapeutic tactics for breast cancer is always selected individually and most often consists of a combination of several techniques.
Modern methods of breast cancer treatment include surgery, chemotherapy and radiation therapy, as well as hormonal and immunotherapy. Therapeutic tactics for breast cancer is always selected individually and most often consists of a combination of several techniques.
Surgical treatment of breast cancer
Surgery is the main treatment for breast cancer. The development of modern medicine makes it possible to perform sparing interventions while maintaining the maximum possible volume of gland tissues. After surgery, radiation and chemotherapy are usually prescribed.
There are several surgical techniques by which surgical oncologists remove tumors:
- radical resection- excision of the area of the mammary gland with lymph nodes and subcutaneous fat;
- radical mastectomy- removal of the entire breast along with lymph nodes and subcutaneous fat. To date, in medical practice, such an intervention is used extremely rarely;
- quadrantectomy- treatment of breast cancer by excising directly the neoplasm with adjacent tissues within a radius of several centimeters. The method is effective in the early stages of the disease;
- lumpectomy is a minimal surgical intervention for breast cancer, involving the excision of the neoplasm and lymph nodes.
Radiation therapy in the treatment of breast cancer in women
 As for the radiation therapy used in the treatment, in case of a malignant lesion of the breast, it can be preoperative, intraoperative, postoperative and independent. The main goal of radiation therapy before surgery is to destroy the maximum number of cancer cells, which allows the tumor to be transferred to an operable state. IN postoperative period radiation therapy is needed to reduce the risk of recurrence.
As for the radiation therapy used in the treatment, in case of a malignant lesion of the breast, it can be preoperative, intraoperative, postoperative and independent. The main goal of radiation therapy before surgery is to destroy the maximum number of cancer cells, which allows the tumor to be transferred to an operable state. IN postoperative period radiation therapy is needed to reduce the risk of recurrence.
In some cases, radiation exposure is used directly during surgery, when the surgeon tries to preserve as much gland tissue as possible. If it is impossible to carry out surgical intervention, radiation therapy is used as an independent therapeutic method. In addition to remote radiation therapy, interstitial radiation therapy can also be used, in which the radiation source is delivered directly to the neoplasm. The lymph nodes are also exposed to radiation.
The medical methods of treating this pathology include chemotherapy, which involves taking cytostatics - drugs that destroy malignant cells. This therapy has many side effects, therefore, its appointment is carried out only in accordance with the regulations and taking into account the patient's condition.
Hormone therapy for breast cancer
 Since breast cancer is triggered by increased estrogen activity, appropriate hormonal correction can be prescribed. It is effective when a woman is diagnosed with a cancerous tumor that has hormonal sensitivity. The methods of hormonal therapy include surgery to remove the ovaries, as well as taking medications that are selected by the doctor on a strictly individual basis.
Since breast cancer is triggered by increased estrogen activity, appropriate hormonal correction can be prescribed. It is effective when a woman is diagnosed with a cancerous tumor that has hormonal sensitivity. The methods of hormonal therapy include surgery to remove the ovaries, as well as taking medications that are selected by the doctor on a strictly individual basis.
When drawing up a treatment plan, the doctor must take into account the type and size of the tumor, the presence of regional and distant metastases, the results of laboratory and instrumental studies, and the general condition of the patient.
A special place in the treatment of breast cancer is given to competent rehabilitation. The therapy of such a serious disease is always associated with psychological and social difficulties, so special attention should be paid to the adaptation of patients. Recovery appearance mammary glands can be used reconstructive plastic surgery. They can be carried out immediately after the intervention to remove the tumor.
Forecast
To date, breast cancer is the most studied of all types of cancer, and detected at an early stage, it is very successfully treated. When compiling an individual prognosis, it is necessary to take into account the anatomical form of growth, size, localization, rate of tumor development, and other criteria.
The most favorable prognosis is noted for hormone-dependent tumors, since the disease in this case has a long pre-tumor period. There are also tumors of the so-called favorable histological type. They are easier to treat than, for example, invasive ductal neoplasms, even if the latter are quite small.
The prognosis of the disease in question is also largely determined by the degree of metastases. Studies show that breast cancer is less amenable to therapy, in which more than four lymph nodes are affected. Regional metastasis in breast cancer is considered the most favorable, in contrast to hematogenous metastasis. The latter form may be indicated by the absence of metastases in the lymph nodes with a tumor size of more than two centimeters. The worst prognosis is noted in the presence of distant metastases. Not less than importance assigned to indicators of tumor markers. If their level is elevated, there is a high probability of tumor metastasis or its recurrence.
survival data
 An indicator of the success of breast cancer treatment is a five-year survival rate, which today is about 55% for this disease. In the absence of adequate therapy, this figure decreases to 10%. Many factors influence the survival prognosis for breast cancer. If we consider the statistics of survival by stages, then in the first stages with a tumor size of less than two centimeters, the five-year survival rate is up to 95%. In the second stage of breast cancer, with a tumor size of up to five centimeters in the presence of malignant cells in several lymph nodes, this figure is about 55-80%.
An indicator of the success of breast cancer treatment is a five-year survival rate, which today is about 55% for this disease. In the absence of adequate therapy, this figure decreases to 10%. Many factors influence the survival prognosis for breast cancer. If we consider the statistics of survival by stages, then in the first stages with a tumor size of less than two centimeters, the five-year survival rate is up to 95%. In the second stage of breast cancer, with a tumor size of up to five centimeters in the presence of malignant cells in several lymph nodes, this figure is about 55-80%.
With the defeat of the lymph nodes and the germination of malignant cells of a large tumor in the skin of the breast at the third stage of cancer, the five-year survival rate among patients is less than 50%. At the fourth stage, in the presence of distant metastasis - up to 10%.
However, if you take care of your own health, undergo regular screening and immediately begin combined treatment when a tumor is detected, the prognosis of the disease can be more comforting. As practice shows, the combination of surgical treatment with chemotherapy and radiation therapy is the most effective in breast cancer. Following the recommendations of a doctor, as well as a healthy lifestyle and diet will help prolong life and maintain health.
Olga Ravilova | 2016-10-28
Breast cancer occurs not only in women, but sometimes in men as well. If breast cells begin to develop uncontrollably and a malignant tumor has formed, then doctors diagnose cancer.
It is important to be able to identify the first signs of breast cancer at an early stage of the disease. Self-diagnosis (knowing how to self-examine the breast) helps detect breast cancer before it spreads throughout the body. Regular mammograms are also helpful.
Self-diagnosis - self-examination of the breast
Self-examination of the breast should be carried out regularly, every month, 5-7 days after the end of menstruation. It is advisable to mark the days in advance on the calendar when you will conduct a self-diagnosis of cancer.
Remember: regular self-diagnosis of breast cancer will help determine and remember the “normal” breast condition.
Set a reminder on your phone or hang a reminder in your bedroom or bathroom so you don't miss your self-diagnosis day. Try to write down all your observations in a diary.
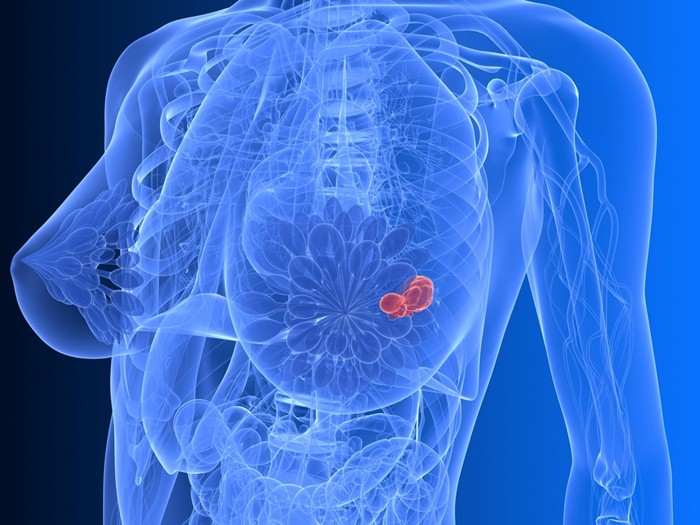
Test in a room with good lighting. The procedure for self-diagnosis of breast cancer is as follows:
1. Conduct a visual inspection To do this, stand with your hands on your hips and examine yourself in the mirror. Assess the size, color and shape of the breasts for any abnormalities. If you have any of the following symptoms, tell your doctor:
 Take a good look at yourself in the mirror. Photo: WikiHow
Take a good look at yourself in the mirror. Photo: WikiHow - Noticeable breast swelling even though you are not currently on your period
- Irregularity, wrinkling, swelling of the skin
- inverted nipples
- Nipple displacement
- Redness, rash or tenderness.
2. Raise your hands and re-examine. 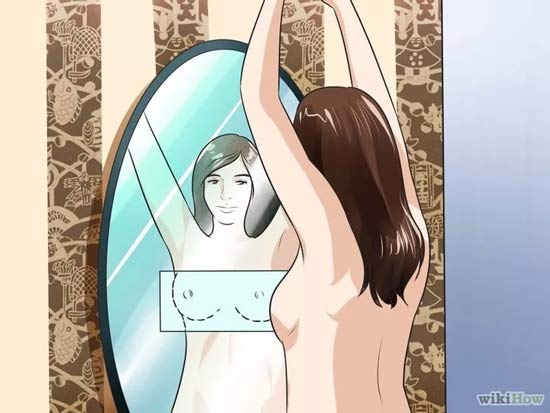 Raise your hands and look in the mirror again. Photo: WikiHow Check for nipple discharge. If there is a discharge, determine its color (yellow, transparent) and consistency (bloody, milky). Pay special attention to the discharge that comes when you are not squeezing the nipple. Also tell your doctor if you have clear or bloody issues or discharge comes from only one breast.
Raise your hands and look in the mirror again. Photo: WikiHow Check for nipple discharge. If there is a discharge, determine its color (yellow, transparent) and consistency (bloody, milky). Pay special attention to the discharge that comes when you are not squeezing the nipple. Also tell your doctor if you have clear or bloody issues or discharge comes from only one breast.
3. Feel the chest.  Feel the chest well. Photo: WikiHow Lie on your back. Bring your index, middle and ring fingers together right hand. Feel the left breast with the pads of the three middle fingers in small circular motions. Their circumference should be 2 centimeters. Feel the chest, moving from the collarbone to the stomach. And then, starting from the armpit, move from the side to the middle. Repeat the above with the other arm and opposite chest. To make sure you've probed the entire area, move in vertical lines. Then stand or sit down and repeat these steps. Walk over the entire surface of the breasts. Many women choose to do this last step in the shower.
Feel the chest well. Photo: WikiHow Lie on your back. Bring your index, middle and ring fingers together right hand. Feel the left breast with the pads of the three middle fingers in small circular motions. Their circumference should be 2 centimeters. Feel the chest, moving from the collarbone to the stomach. And then, starting from the armpit, move from the side to the middle. Repeat the above with the other arm and opposite chest. To make sure you've probed the entire area, move in vertical lines. Then stand or sit down and repeat these steps. Walk over the entire surface of the breasts. Many women choose to do this last step in the shower.
- Check for lumps or other changes. Tell your doctor about any lumps you find.
- The chest should be felt with light, medium and strong pressure with each circle. In other words, feel for a small circle with light pressure, and then re-traverse the same area with medium to hard pressure. Light pressure helps to detect tissue changes near the surface of the skin. Medium pressure allows you to feel the deeper tissues, and the strongest pressure helps to reach the deepest tissues near the ribs.
It should be remembered that the results of self-diagnosis are contradictory. Some studies show that self-diagnosis does not increase the likelihood of cancer detection. Talk to your doctor about breast cancer self-diagnosis. Your doctor may recommend that you carefully examine your breasts so that you can notice changes if they occur.
Risk Factors for Breast Cancer
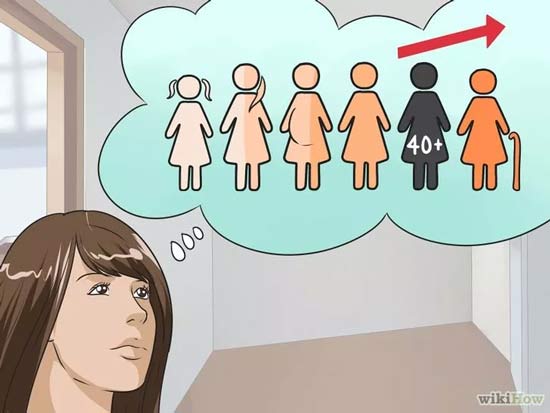 The risk of getting breast cancer increases after age 40. Photo: WikiHow
The risk of getting breast cancer increases after age 40. Photo: WikiHow It is vital to detect breast cancer at an early stage, especially if you are exposed to risk factors for cancer: there is a genetic predisposition, you are over 40 years old, there are lumps on probing. If in doubt, a mammogram should be done.
- If anyone in your family has had breast cancer, gather detailed information that can help your doctor, such as the type of tumor (primary or secondary), treatment or surgery performed, response to treatment, and outcome.
- Sometimes treatment started just a few weeks early can save a person's life. Don't put off testing until later.
 Some people are genetically predisposed to breast cancer. Photo: WikiHow
Some people are genetically predisposed to breast cancer. Photo: WikiHow Be aware of genetic predisposition. Women are more likely to develop breast cancer than men. In addition, if any of your close relatives (eg mother, sister) had breast cancer, you are more likely to develop breast cancer. There are also inherited gene mutations that predispose a woman to an increased risk of breast cancer. These gene mutations are BRCA1 and BRCA2. Five to ten percent of breast cancers are caused by these gene mutations.
- Caucasian women are most at risk of developing breast cancer.
- Some ethnic groups more prone to mutated BRCA genes. These include people of Norwegian, Icelandic, Dutch and Jewish descent.
Many diseases that you currently have can affect your chance of developing breast cancer. Certain illnesses can affect your risk of breast cancer. Women who already had cancer in one breast are more likely to develop cancer again.
 Some diseases contribute to the development of cancer. Photo: WikiHow
Some diseases contribute to the development of cancer. Photo: WikiHow
People who are in childhood were exposed to radiation in the chest area, also have an increased likelihood of developing a tumor. In addition, other medical facts, such as starting your period at age 11 or earlier, may increase this risk.
Starting menopause later than normal can also be a cause for concern. If a woman is on hormone therapy after menopause or has never been pregnant, it also increases her chance of developing breast cancer.
Lifestyle strongly influences the predisposition to breast cancer. At risk are obese people, smokers and drinking people. For example, women who drink more than three times a week increase their chances of getting breast cancer by 15%, and smokers who start smoking before the birth of their first child are at a special risk zone.
Prevention of breast cancer
 Prevention of breast cancer is very important. Photo: WikiHow
Prevention of breast cancer is very important. Photo: WikiHow The increase in the number of cases of breast cancer indicates the need for preventive measures aimed at reducing the risk of the likelihood of the disease. To reduce the chances of getting cancer, you need to regularly visit a gynecologist, a mammologist (do a mammogram), constantly monitor your breasts, and change your lifestyle to a healthier one.


Visit your gynecologist annually. During your annual gynecological exam, your doctor will examine your breasts for lumps or abnormalities. If your doctor finds anything unusual, he will recommend a mammogram.
If you do not know where to turn for help, contact your local clinic, a local therapist. Your therapist will refer you to the appropriate specialist, depending on your situation. You may get a mammogram for free or inexpensively.
Breast cancer is still the most common disease in women today. Approximately 20,000 patients per year still die as a result of this disease. Many of them could get a chance for recovery if breast cancer could be detected in a timely manner.
Early diagnosis is important, because the chances of treatment and recovery are greater, the smaller the tumor at the time of its discovery. The tumor, determined by touch, as a rule, already has a size of about 2-3 cm.
The goal of early diagnosis is to detect breast cancer already at the stage when the tumor is still small size and is not palpable.
Women should not wait until they discover a lump in their breasts on their own. Since at present there are numerous diagnostic methods that make it possible to detect breast cancer and even its initial signs - and even before the moment when the seal is palpable and, as a result, turns into a life-threatening disease. These include digital mammography, sonography and MRI (magnetic resonance imaging).
However: despite advances in the field of medicine, methods of early diagnosis of the disease in Germany are still reluctantly used. According to the provisions of the early diagnosis of cancer, women under the age of 50 are still recommended only to independently examine the breast by probing and visit a gynecologist for the same purpose. And this despite the fact that it is known that when a seal is felt in the chest, the disease is already progressing. Thus, palpation of the breast is actually not a way of early diagnosis of the disease, but rather "its late detection."
2. How does breast cancer occur?
Breast cancer is not always like this.
The cause of this disease in most cases (about 80 percent) are cells that envelop the milk ducts from the inside. Here they go through a phase during which they are finally fixed in the milk ducts, the walls of which "encapsulate" them. At this stage, the tumor cells have not yet spread throughout the body. This phase is called "in-situ-stage", the first stage of breast cancer, that is, "ductales Carcinoma in-situ" or "DCIS" for short. During this phase, the cancer always and in all cases curable. Since at this stage there is no formation of seals, and changes occur only in the cells, it is almost impossible to determine the signs of the disease by touch. Altered in this way, cells of the breast lobes (in about 20 percent of women) do not necessarily develop into breast cancer, however, they are called "Carcinoma lobulare in situ" or "CLIS" for short.
After some time, these cells from the milk ducts penetrate into the tissues of the breast. This process is called " invasive cancer. This tumor (the "real" breast cancer) is also treatable, as long as it is only in the breast. But when cancer spreads through the bloodstream throughout the body and tumor metastases penetrate into vital organs, it is no longer possible to cure it. In any case, it can go into a chronic stage or, in the worst case, quickly lead to death. Therefore, the goal of early diagnosis of breast cancer is to detect the disease when it has not yet spread throughout the body. Or better yet, identify the disease before it can become dangerous - namely the first stage (DCIS).
Early detection of breast cancer means an increased chance of recovery!
Breast cancer is curable if detected early. Thus, early diagnosis of the disease means:
- Detect disease before a palpable lump forms in the breast.
- Timely diagnose the disease in order to prevent its transition to an aggressive tumor at an early stage of the process.
You need to know:
- It is impossible to determine the disease at the initial stage by feeling the breast, since not every type of breast cancer entails the formation of seals. This means that breast examination by palpation is the crudest method for detecting cancer and can detect only those tumors that are palpable (usually lumps larger than 2 cm.)
- Ultrasound examination of the mammary glands is also not able to detect breast cancer at an early stage.
3. What diagnostic methods exist?
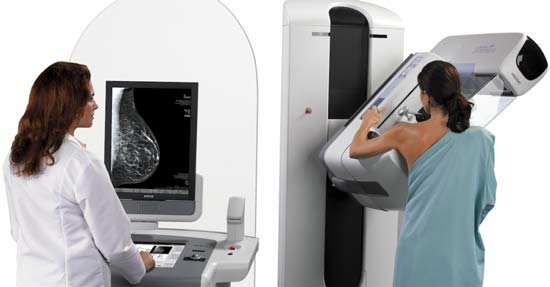
Mammography
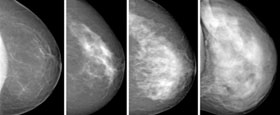
Mammography allows early detection of the disease (DCIS), because in some cases (about 30 percent) slight traces (so-called "microcalcifications") are visible on the x-ray. Such microcalcifications occur mainly in the presence of slowly developing tumors of the lactiferous ducts, while rapidly developing DCIS tumors are rarely accompanied by microcalcifications. These stages of rapid development (in about 70 percent of cases) are more often detected using magnetic resonance imaging of the breast. About two-thirds of cases of the disease are not detected during mammography, since microcalcifications are not visible on the mammogram.
In addition, mammography alone for diagnosing cancer at an early stage is not suitable for all women. When the breast tissue is still very dense, larger tumors may also not be detected. Reason: Breast tissue on mammography white color just like breast cancer itself. Only after the breast tissue is docked and replaced with fatty tissue, the reliability of mammography increases. For some women, this happens with age, for some, on the contrary, never. Thus, for each woman there is a certain level of accuracy in diagnosing breast cancer through mammography, it depends on the "density" of the breast tissue.
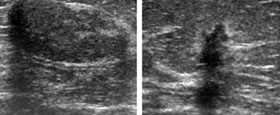
Sonography
Sonography(Breast Ultrasound) is an important adjunct to mammography especially for women with fully developed breast tissue. Through ultrasound, the doctor can "look" into the dense tissue of the breast and detect cancer when it is impossible to do with a mammogram. In addition, benign cysts can be detected in this way. Ultrasound also shows changes in breast tissue and cancer-like growths that cannot be detected by palpation. However, only ultrasound or the so-called "3D sonography" is not intended for early diagnosis of the disease. Reason: It is impossible to accurately diagnose cancer at an early stage with ultrasound. Ultrasound is an important complement to mammography, especially when the examination is performed by an experienced specialist. But it cannot replace a mammogram.
Magnetic resonance imaging based on nuclear magnetic resonance (MRI)
MRI, like ultrasound, is a method of examination without the use of x-ray radiation. However, unlike ultrasound, MRI can detect cancer at an early stage. A particularly strong diagnostic side of MRI is that it detects biologically aggressive cancers at an early stage based on increased blood flow - especially in those initial stages that are in a hurry to form microdeposits, by which they can be detected on mammography. At these stages of cancer, as well as in the presence of aggressive invasive carcinomas that are their consequence, mammography is as "blind" as in the examination of mammary glands with dense gland tissue. However, the same rule applies to MRI: the method is most convincing only when the technique, technique and especially the experience of the doctor are at the appropriate level.
Each method has its limits - so it's about the right combination!
This means that no examination technique (mammography, sonography or MRI) used without additional methods can detect all types of cancer at an early stage. Each individual method has its own purpose in the process of diagnosing breast cancer, so it is important to combine them correctly. Which combination is appropriate for you depends to a large extent on your age, your breast tissue characteristics, your breast density, your personal risk profile and your individual need for a reliable diagnosis.
![]()
- Mammography all women should fundamentally consider the basis of early diagnosis of the disease, it also contributes to the detection of breast cancer in the early stages.
- Sonography complements mammography where x-ray alone is not sufficient.
- Holding MRI milk jelly makes sense if your family has already had cases of breast and / or ovarian cancer. In addition, MRI is also the most accurate way to diagnose the disease in women with dense breast tissue. It is most reliable in detecting biologically aggressive cancers in the early stages. It most reliably detects the presence of breast cancer and cells with biologically aggressive potential.
Combining different diagnostic methods increases disease detection rate compared to using just any single method.
4. Screening mammography is just the first step
Breast cancer is not always the case, so mammography screening is not suitable for every woman.
All mammary glands are different. Therefore, breast cancer in each woman manifests itself differently. Inexpensive standard methods, such as screening mammography, cannot replace the individual method of early detection of breast cancer, which you, as a woman, should use. Since in order to match the diagnostic method to your individual risk factors and prevention needs, a multi-step, clear diagnostic process is necessary, which, after consultation with an experienced specialist, will allow you to combine different examination methods in order to make an accurate diagnosis. Therefore, screening mammography, which in question is only the first step in the diagnosis.
As part of screening mammography, two x-rays of each breast are taken, without prior medical examination or identification of your individual risk profile, which are then evaluated by two specialists. The conclusion of doctors are reported in a few days. If the “diagnosis” column says “mammographic examination without pathology”, this means that mammography did not reveal any pronounced changes. Since a mammogram cannot detect all types of breast cancer, this phrase does not necessarily mean that your breasts are healthy. In addition, you will not be able to find out at all whether it is possible to detect a disease in your mammary glands at an early stage only through mammography.
By the way: In 75% of cases, breast cancer is not detected through screening mammography.
Mammography screening is performed exclusively in women aged 50 to 69 years. Although among the representatives of this age group breast cancer is no longer as common. Increasingly, women under the age of 50 are affected by this disease, and they often have aggressive and rapidly growing tumors. For women in this age group, as well as for those over 69 years of age, early diagnosis of the disease is not possible using the method with visual results. But if the presence of a tumor was discovered too late, for example, because a woman discovered them through a self-examination by probing, then the chances of recovery are reduced.
5. AIM works for you.
Women need a personalized method for detecting breast cancer at an early stage.
Committee for Individual Breast Cancer Diagnosis (AIM e.V.) is an association of doctors, patients with breast cancer, as well as women who do not have this disease, who want to support the association of individual early diagnosis of breast cancer. The aim of AIM is to provide in Germany an individualized and risk factor-oriented early diagnosis of breast cancer by using all methods with visual results today and in the future.
AIM doctors want to provide women of all ages with the opportunity to detect cancer at an early stage and further treat the disease using diagnostics that meet the highest international quality standard. In this case, the main thing is the method of diagnosing the mammary gland, taking into account the individual risk profile of each woman, as well as personal medical advice regarding the possibilities of prevention and methods of treating the disease. Because only in this way, in contrast to the standard and anonymous screening procedure, it is possible to achieve the optimal result for each woman.
Breast MRI Quality Certificate
Breast MRI: Association for Personalized Breast Diagnostics (AiM) develops quality certificate
Breast MRI as a standard method for early detection of breast cancer - yes or no? The answer to this question has now been proven through numerous scientific studies, including by Christiane K. Kuhl and Wendy Berg, quite and convincingly: Thanks to technical and methodological progress, magnetic resonance imaging of the mammary glands is today one of the most informative methods in the diagnosis of breast cancer.
Critics who are now refusing to use breast MRI still cite the often erroneous positive and negative conclusions as "an undeniable argument." This overlooks the following: according to the experience of Prof. Uwe Fischer and Prof. Christiane Kuhl, chairpersons of the Association for Individual Breast Diagnostics, the problem is not the examination method itself, the reason for the erroneous conclusion is rather the lack of personal qualifications, as well as the lack of the necessary technical equipment in medical practices and clinics. The consequence of this is significant differences in quality when examining and evaluating MRI of the mammary glands.
The breast MRI quality certificate, which was developed by the association for individual breast diagnostics (AiM) under the direction of Prof. Uwe Fischer and Prof. Christiane Kuhl, should help ensure the quality of breast cancer MR imaging throughout Germany. In August 2010, the Diagnostic Center for Breast Diseases in Göttingen was recognized as the first center according to the AiM level 2 standard (expert level) by the Department of Technical Control for Radiation Protection. Radiology Clinic Rhenish-Westphalian technical university The city of Aachen (RWTH) will also soon be certified as the first "expert level" university center.
The certificate is issued at 2 different levels: “Breast MRI at a high level” and “Breast MRI at an expert level”. Medical practices and clinics that acquire this certificate must certify the availability of certain equipment, in addition, a minimum number of examinations (for a high level, this is at least 250 diagnostic breast MRI scans per year, for an expert level, 500 diagnostic breast MRI examinations and more than 100 MR-guided interventions). Obtaining a certificate, according to Professor Fischer, will significantly increase the incentive for breast diagnosticians to upgrade equipment and improve the quality of assessment. “In addition, this certificate provides for transparency between doctors and women in need of treatment,” says Prof. Fischer. “This will lead, in the medium term, to focusing research with proven expertise on peers with expert certification and that the number of researchers with high expertise will increase in the long term.”
Modern breast diagnostics: Data - Facts - Concepts.
Epidemiology
Breast cancer is the most common malignant disease in women in the West. During her lifetime, one in nine women - according to the latest data from the Netherlands, even one in eight women - will develop breast cancer. In Germany every year about 56,000 women are diagnosed with
"mammary cancer". The share of breast carcinoma in women is 38 percent of new cases of cancer. Among women aged 40 to 50 years, breast carcinoma is the most common cancer. In Germany, nearly 18,000 women with a confirmed diagnosis of breast cancer die each year. Compared to EU countries, Germany is in the middle of the ranking of breast cancer deaths, as well as new cases of cancer. Recently, probably as a consequence of the regression of hormone replacement, in line with the trend, the incidence of breast cancer has been declining. However, the age at first diagnosis continues to decline.
Early detection of the disease as a rational medical strategy
The prognosis of breast cancer largely depends on the size of the tumor, the aggressiveness of the tumor, and the stage of the disease. If we are talking about the time of diagnosis and the disease is limited to the breast (without lymph node involvement and distant metastases), then currently about 97 percent of cases have a survival time of 10 years. If the cancer has already spread to the axillary lymph nodes, then the 10-year prognosis drops to less than 80 percent. In the presence of distant metastases, the survival rate drops sharply to below 30 percent. The task of diagnosing breast cancer is to identify the disease at an early stage, if possible limited only to the mammary gland.
Research methods in the diagnosis of the breast
For this purpose, along with inspection and palpation, medical imaging techniques such as mammography, breast ultrasound, and breast MRI are available. If any abnormalities are found during the diagnosis, then it is possible to conduct a percutaneous histological analysis in the form of a puncture or vacuum biopsy.
Clinical researches
The clinical examination, along with the collection of anamnestic data, includes examination and palpation of both breasts. On examination, skin tightening and nipple retraction or inflammatory changes may be detected, which may indicate malignancy. During palpation, it is worth paying attention to the density and formation of nodes. According to research data, there is of course no guarantee that a reduction in mortality among women in the 40 to 69 age group can be achieved through self-examination. It also highlights the implementation of the current directive S3: “Breast self-examination, even with regular use and training, being the only method, is not able to reduce the mortality rate from breast cancer.” However, women who self-examine regularly are more healthy lifestyle of life show a better "awareness of the condition of their breasts". That is why medical professional associations continue to recommend self-examination of the chest, although a palpation examination does not actually detect the disease at an early stage.
X-ray mammography
X-ray mammography is currently used as the main method of medical imaging for the early detection of breast carcinoma. The areas of mammography are the determination of microcalcifications and the detection of lesions in areas of adipose tissue caused by tumors. The content of x-ray mammography, however, varies greatly depending on the density of tissue in the breast. Currently, four types of mammogram density are distinguished, depending on the corresponding proportion of adipose and glandular tissue (ACP Type I-IV; ACR = American College of Radiology). In women with low tissue density (predominantly lipomatous tissue, AKP density type I), mammography has achieved a high degree of confidence in the detection of breast cancer. In women with involutionally developed breasts (AKP density types 3 and 4), the sensitivity of mammography is reduced to below 40 percent. Because of these severe limitations, women with inhomogeneous dense or extremely dense parenchyma on mammogram (AKP III, AKP IV) are advised to use a second type of medical imaging (eg, ultrasound, breast MRI) for diagnosis.
Currently for research female breast increasingly using digital technologies. In doing so, it is necessary to distinguish between "digitized" mammography and true digital full-fledged mammography. If the first type is accompanied by a higher radiation dose compared to conventional ("film") mammography (!), then the radiation dose for wide-field mammography can be reduced compared to conventional diagnostics - with a significantly higher diagnostic certainty.
Mammography is usually carried out in the form of a so-called two-plane mammography. At the same time, the study depicts two standard planes - with an oblique mediolateral ray trajectory (SML) and with a craniocaudal ray trajectory (CC). The criteria for good system tuning and defect-free image quality cover the so-called four-stage PGMI system(PGMI = excellent, good, moderate, insufficient), or the three-stage system used in Germany.
Mammography results are described according to the so-called "BI-RADS Lexicon" of the American College of Radiology (BI-RADS = Breast Imaging Interpretation and Recording System). At the same time, 3 main results of the study are determined and described: foci / seals, calcification and violation of architectonics.
After analyzing the image and describing the results of the study, the categorization of x-ray mammography is mandatory. The description of BI-RADS report categories can occur in stages 0, 1, 2, 3, 4, 5, or 6, with additional subdivisions of category 4 into subgroups 4A, 4B, and 4C. The BI-RADS categorization expresses how likely a malignant lesion is. In addition, recommendations on how to proceed further follow from the BI-RADS categorization.
Breast ultrasound (breast sonography)
Breast ultrasound, along with mammography, is the most widely used medical imaging method in breast diagnosis. The method is biologically safe. sound waves, which are sent to the breast tissue and whose echoes are received, lead to the visualization of intramammary structures. The decisive factors are the mechanical properties of the tissue, such as density and sound velocity, which differ especially in adipose tissue, connective tissue and calcifications. If these components appear close to each other, as in heterogeneous glandular tissue, then echogenicity increases. Since only one constituent tissue usually predominates in tumors, "dark spots" are depicted and therefore, in the light environment of the gland, they are usually better delineated than in mammography. Other possibilities arise in dynamic analysis with checking the elasticity and mobility of space (from the point of view of ultrasound). Thanks to the technology that allows you to view images in a section, you can better determine deep-lying structures and processes occurring at the periphery. Additional information can be obtained using Doppler sonography through an assessment of the degree of vascularization of the changes. Ultrasound is limited by the poor spatial resolution of microcalcifications, which still represent the area of mammography.
Due to the individual and manual control of the ultrasonic transducer, this method is not well standardized. Breast ultrasound is therefore determined, along with the quality of the equipment, to a decisive extent by the skill and experience of the examiner. The examination time depends on the size of the breast, the evaluative capacity of the tissue, and the number of dependent examination results. As a rule, this procedure lasts from 3 to 5 minutes on each side, but in difficult cases the duration can increase to more than 15 minutes.
Suitable for breast ultrasound are only linear transducers with high resolution and an average frequency of ≥ 7 MHz. If the frequency is too high, the evaluative ability may deteriorate again. Although at a carrier frequency > 13 MHz high definition in the superficial area, however, deeper tissue layers will not be sufficiently imaged with such a sensor. In general, high frequencies need to be adjusted to explore the required penetration depth. Broadband transducers that cover a wide range of frequencies are the best solution to this problem. The disadvantage of high resolution transducers is the limited image field width (typically 3.8 cm). Modern devices, however, have at their disposal an electronic trapezoidal scanner, which allows you to set the image field width > 5 cm in depth when examining large breasts.
Areas of application for breast ultrasound include:
- initial diagnosis of asymptomatic young women,
- principal use for diagnosing symptomatic women
- punctures, which are carried out under ultrasound control, and
- complete diagnosis of women with a dense tissue structure during mammography.
The main aims of ultrasound are to detect and, in particular, characterize changes in the breast when breast carcinoma is suspected. There are a number of differential diagnostic evaluation criteria for this, which have been described in detail in the BI-RADS lexicon and by the German Society for Ultrasound in Medicine (DEGUM).
Based on the categorization of the X-ray mammographic results of the study, ultrasound is evaluated in accordance with the seven-level BI-RADS system (ultrasound system-BIRADS. 0, 1, 2, 3, 4, 5 and 6). The results resulting from the respective ordering are identical to those of mammography.
Breast MRI (magnetic resonance imaging of the breast)
X-ray mammography and ultrasound of the breast allow to obtain an image of intramammary structures of the tissue through the characteristics of the tissue absorbing x-rays or reflecting ultrasonic waves. In contrast, during magnetic resonance imaging (MRI), the detection of malignant tumors of the breast occurs due to the display of increased vascularization.
Data over the last 10 years clearly show that breast MRI is the most sensitive method for detecting breast cancer, both for ductal tumors (DCIS) and for invasive cancer.
Excellent results of breast MRI can only be achieved if there is a high technical and methodological quality and high professionalism of the doctor. It should be noted that today there is no guarantee of the quality of magnetic resonance studies, and that at present the current applicable benefits of the association of physicians are far from reflecting modern research methods.
Breast MRI analysis takes into account morphological criteria and those relating to contrast enhancement. The usual scoring scheme describes the abnormal results of studies, including shape criteria, delimitation, distribution, as well as the initial and subsequent signals after the administration of a contrast agent. In the results of MRI studies, the fundamental difference between the focus (< 5 mm), очаговыми поражениями (объемного характера) и необъемными («немассивными») поражениями.
The use of MR mammography is always appropriate when other examination methods provide unclear results or indicate limitations. This usually occurs as part of pre-treatment in case of detection of breast cancer, and even in cases of invasive carcinoma detected on ultrasound or mammogram, and in women with microcalcifications in whom ductal carcinoma in situ is suspected, or, for example, if cancer confirmed by mammogram-guided vacuum biopsy. This is important because ductal carcinoma in situ (DCIS) is often accompanied by incomplete calcifications, so the true extent at the time of mammography may be underestimated.
Since MRI can directly detect ductal carcinoma in situ (i.e., detection of ductal carcinoma in situ does not depend on the presence or absence of calcifications), this allows more accurate actual examination results to be provided. MRI is also used to enhance follow-up after breast-sparing surgery, to detect primary tumors in situations of unknown primary tumor location, or to monitor patients during pre-chemotherapy. In principle, breast MRI can be aimed at solving diagnostic problem cases (for example, when there are several ambiguous findings in patients with high-density breast mammography).
MR mammography is particularly important for early detection. MRI is especially useful in examining women at high risk of developing breast cancer. These include women with a detected pathogenic mutation in the breast cancer gene or women whose families had frequent cases of breast or ovarian cancer (for example, 2 or more cases in the same line, especially at the age of the disease< 50 лет). В основном ежегодно рекомендуется проходить МРТ для раннего обнаружения в более чем 20 %, начиная с возраста потенциального риска заболевания. Имеет смысл использовать МРТ в качестве дополнительного метода раннего обнаружения заболевания у женщин, у которых были получены результаты гистологического исследования, и которые относятся к категории женщин с повышенным риском развития рака молочной железы. К ним относятся женщины, у которых оперативно обнаружен дольковый рак молочной железы in situ или атипичная протоковая гиперплазия. Наконец, ежегодное обследование МРТ для раннего выявления болезни имеет важное значение для женщин, которые находятся в группе повышенного риска развития рака груди, из-за получения так называемого «полного облучения лимфатических узлов» для лечения лимфогранулематоза (лимфомы Ходжкина). Все раннее проведённые исследования по теме «Использование МРТ для раннего обнаружения болезни у женщин повышенной группы риска развития рака молочной железы» единогласно подтверждают, что эффективность МРТ в выявлении рака молочной железы (инвазивного или внутрипроточного) значительно выше, чем при маммографии. Со значением эффективности обнаружения от 90 до 95 процентов, МРТ примерно в два-три раза выше, чем маммографии (30 — 40 процентов). Даже при комбинированном использовании маммографии и УЗИ эффективность обнаружения повышается только до около 50 процентов — что доказывает, что даже дополнительное использование УЗИ не может заменить МРТ.
When diagnosing women with normal, not elevated risk of the disease, MRI is rarely used today, primarily in terms of costs. Because the lower the overall incidence of breast cancer, the more healthy women need to be screened for additional carcinoma by MRI. However, all previous data indicate that the "sensitivity gradient" between MRI and mammography is largely independent of the woman's morbidity risk. This means that even for women at normal risk of the disease, MRI is more accurate than mammography and ultrasound. However: very rarely, but there are such cases that with a low incidence rate, a malignant tumor is not visible with the help of mammography and ultrasound, and it is detected only with the help of MRI.
A condition for the use of MRI for diagnosis in women at normal risk of disease is that the MRI must be performed by an experienced specialist and that minimally invasive biopsy techniques are available. There are a huge number of women who are interested in early detection of breast cancer using MRI, they need to be informed about the pros and cons of such an intensive method of early detection of the disease: about the limitations of MRI, the need for additional mammography diagnostics (MRI does not replace mammography), and about possible false positive diagnosis and its consequences.
Analysis of favorable MRI images leads to a mandatory final classification of the overall results of the study according to the seven-point scale of the BI-RADS system (MRM-BIRADS 0, 1, 2, 3, 4, 5 and 6). After the assessment by the MRM-BIRADS system, an assessment takes place, taking into account the results of other research methods, for the overall assessment of studies according to the BIRADS system.
Biopsy (percutaneous biopsy method)
BIRADS category 4 or 5 results should be clarified primarily by percutaneous biopsy and verified by histological analysis. The relevant study results should not normally lead to this kind of inadequate primary therapy (eg, surgery). There are two methods for percutaneous ambulatory biopsy. The first method is a needle biopsy, with the help of which three to five tissue samples can be taken at high speed. This method is preferably used in ultrasound-guided intervention. The second method is a vacuum biopsy, with the help of which pieces of tissue are taken in the form of cylinders, on average 20 gauge. The vacuum method is usually used for stereotaxic examination of microcalcifications using MR-guided biopsy. Fine needle puncture is used to sample symptomatic cysts or prominent axillary lymph nodes.
The biopsy should be performed under the guidance of a specific medical imaging technique that shows the most pronounced conditions, it should be noted that ultrasound-guided interventions are easier to handle than stereotactic biopsy. MR biopsy is expensive and is only applicable when other studies cannot clearly show relevant relationships.
Conditions that require surgical intervention, which are hidden, should be noted for the surgeon before the operation. This applies primarily to pronounced microcalcifications, but also to non-palpable disturbances in architectonics and foci. As a rule, such localization mark with a thin wire, which is placed at the site of the intended removal or in the region of characteristic target points. Marking is also done by introducing staples or curls. Before surgery, especially in the presence of microcalcifications, it is required to make samples necessary to witness complete removal and, possibly, re-extraction.
Concepts for early detection of breast cancer
For the early detection of breast cancer, many specialist societies recommend the regular use of X-ray mammography from the age of 40, since in this way there is a possibility of increasing survival among the women examined. The interval between surveys in the data is typically one to two years.
Classical screening mammography is a comprehensive mass examination, for example, in Germany, women aged 50 to 69, even if they are asymptomatic, are invited to undergo X-ray mammography every two years. Clinical research, ultrasound and MRI are not used as priority measures. Mammography evaluation occurs twice after a certain period of time. The percentage of repeat applications (percentage of women undergoing a repeat examination) with unclear results of the examination according to European guidelines should not exceed 7 percent (later 5 percent). When re-referring women with inconclusive test results, the physician responsible for them determines how to proceed.
Experience with mammography screening programs in others (including the UK, Canada, the Netherlands, Norway) reaches over 30 years. In countries that did not have adequate mammography infrastructure prior to the introduction of screening (such as the UK), mortality rates have been shown to be reduced by up to 30 percent with the widespread concept of a study invitation. Germany offers other conditions for comparison, since for more than 30 years there has been a so-called gray screening, with about 30 percent of women participating. In Germany, there is still no evidence of a potential reduction in mortality due to screening mammography. Data from other countries also show that, in particular, small tumors can be detected during screening during a mass study. Of course, in the aggregate of all screening concepts, interval carcinomas are fixed in the order of 25-35 percent.
Concepts for individualized and risk-adapted early detection of breast cancer unlike screening programs, they are guided not by the data of the address table (the criterion for selecting and inviting women is the date of birth), but by the specific risk profiles and individual circumstances of women. This includes individual detection of a potentially increased risk of developing breast cancer (eg, familial predisposition, pathogenic mutations in the breast cancer gene, histologically confirmed borderline lesions, tissue density on postmenopausal mammography), as well as individual application of diagnostic imaging techniques, depending on the specific tissue density on the mammogram.
Unpublished data show that, using individualized and risk-adapted concepts, it is possible to increase breast cancer detection rates from 6 ppm to over 10 ppm. At the same time, it is possible to reduce the number of unnoticed carcinomas to less than 2 percent. It should be noted that such modern concepts lead to an increase in costs compared to classical mammographic screening, due to the combined use of various research methods (mammography, ultrasound, MRI).
Critics of this method of early detection of the disease state that ultrasound and MRI are not recommended for early detection in women without an increased risk of developing breast cancer. Because there was no data from prospective selective studies that showed that the additional use of these methods leads to a reduction in mortality from breast cancer, compared with early detection only with mammography.
In addition, the following should be noted:
Early detection through mammography is one of the most studied preventive measures in modern medicine. Its effectiveness in reducing mortality based on prospective randomized trials is fairly well proven. Just because this is the case, it is not necessary to repeat the whole process for each additional breast diagnostic method - but we can and should build on what was created exclusively for early mammographic detection.
The mortality reduction effect of complementary non-mammographic early detection methods can be predicted based on the known mortality reduction effects of mammography and on the difference in cancer detection rates between mammography and combined early detection methods. In short, the benefit of additional early detection methods can be regarded with sufficient safety also in relation to the reduction of mortality in accordance with the principles of evidence-based medicine.
In the concept of early detection of breast cancer in high-risk women (for example, a detected pathogenic mutation of the BRCA1 or BRCA2 breast cancer genes or women with a risk of heterozygote detection ≥ 20 percent, or with a lifetime risk of disease ≥ 30 percent with an uninformative genetic test) begin self-examinations, palpation examinations by a doctor, ultrasound and MR mammography starting at the age of 25 years or five years before the age of the earliest disease in the family. From the age of 30, an additional mammogram is recommended.
Clarifying the diagnosis of symptomatic patients
If you have a symptom that indicates breast cancer, you must definitely undergo a mammogram (the so-called medical mammography) if the patient has reached a certain age (about 40 years). The primary diagnostic method for young women is breast ultrasound.
To confessions (the so-called justified testimony) for such therapeutic mammography are in accordance with the orientational medical care:
- increased familial predisposition
(1 breast tumor among first or second degree relatives, 2 breast tumors among third and fourth degree relatives, ovarian cancer among first degree relatives)
- Palpable nodules, inconclusive palpation results, positive ultrasound
- Unilateral mastodynia
- Histologically determined risk of lesions (eg, atypical intraductal hyperplasia, radial scarring, lobular carcinoma in situ)
- Discharge from the nipple
- Condition after surgery to remove breast cancer
- Inflammatory changes, mastitis, abscess
- Newly diagnosed nipple or skin changes
If there is at least one of the above signs, it is recommended to undergo an examination that, with the greatest possible certainty, will exclude or still confirm the presence of a malignant diagnosis.
Such clarifying diagnostics cannot be carried out in accordance with the legal provisions in screening centers that are designed for early detection of the disease in healthy women, because they can only offer one method of research - a mammogram.
Diagnosis of breast cancer by imaging
As part of follow-up after breast cancer, diagnosis is made by imaging for women who have undergone breast-conserving treatment, twice a year for three years of the operated breast, and once a year of the opposite breast. After three years, an annual interval is recommended for both breasts. Regular follow-up MRIs are not considered if an MRI is performed prior to surgery and partial removal has been performed, then there is no need for an MRI for the first three years. Then, after the mammogram, an individual decision is made on the need for an additional MRI study for follow-up.
A major problem in dispensary care for patients in the convalescent phase is the increased risk of breast cancer (meaning that there is an increased risk of recurrence ipsilaterally and also an increased risk of new disease contralaterally) due to degraded mammographic and ultrasound accuracy. Surgery and, moreover, radiotherapy leads to scarring and other accompanying changes (eg, calcification, subcutaneous fat necrosis) that can both mimic breast cancer recurrence and mask it and therefore cause both a false positive and a false negative. diagnosis. Therefore, these women should be referred for additional MRI examinations.
Systematic search for distant metastases is not recommended at this time - but such reasoning is likely to be associated with cost. Regular follow-up through the use of abdominal ultrasonography, if necessary CT, is also useful for the early recognition of metastases in adjacent organs, and is increasingly appropriate given the developments in last years more and more targeted therapies that, in early metastasis, provide effective treatment. These include a number of new systemic chemotherapy methods, as well as local methods of treatment, such as the destruction of liver or lung metastases using radio frequencies, transarterial radioembolization of liver metastases.
To us. We will prepare an individual offer for you, taking into account your diagnosis and needs.
Malignant tumors of the mammary glands occupy a leading position among all oncological diseases. The disease of this type develops mainly in women, but cases of its occurrence in men have been recorded repeatedly.
An important task for every person is timely and accurate breast cancer diagnosis. Innovative equipment and high skills of oncologists make it possible to identify the disease on early stages which significantly improves the chances of a full recovery.
Why is breast cancer diagnosed?
The main goal of diagnostic measures is to identify a malignant process. Due to the special location, the disease can be detected at an early stage. Standard manual control of the breast allows you to immediately identify the seal. To confirm the preliminary diagnosis, the specialist additionally conducts mammography and radiography.
You can determine the tumor by feeling the chest. To avoid aggravating the situation, oncologists recommend visiting a mammologist once a year. Additional techniques in the form of radiography are carried out regularly after the age of 35 years. For young women, the procedure can be harmful.
Diagnosis by ultrasound determines the type of cancer, its structure and contours. Ultrasound is an accurate technique by which a malignant lesion can be distinguished from a cyst. Based on the results of the instrumental examination, the specialist appoints. Its feature is the taking of material by the puncture method from the resulting tumor for further examination. The procedure determines the type of cancer and allows you to choose the optimal treatment regimen.
The contribution of competent diagnostics in determining cancer is undeniable. Modern differential and instrumental techniques detect the disease at any stage.
How to diagnose breast cancer yourself
Feeling can be carried out independently at home. This procedure is mandatory. In fact, every woman should perform it with a certain frequency. characterized by the presence of seals and nodules. You can feel them around the entire circumference of the mammary glands. The tumor is characterized irregular shape, the lack of precise contours and a bumpy surface.
Self-diagnosis is carried out every month after the end of menstruation. You need to feel the chest clockwise from the outside to the inside. During the examination, the woman takes a standing position, while the arm (first the left, then the right) is thrown back behind the head.
Warning signals are a wound surface that resembles an ulcer, and pain with clear localization. A bad sign is also considered the presence of deformation of the contour of the chest and the appearance of depressions.
One of the signs of cancer is the presence of "retraction" of the nipples. Peeling of the skin around them and the presence of secretions are not excluded. A serious sign of a developing disease is the appearance of limited ulcers, bruising and redness.
Malignant tumors often metastasize, mainly to the lymph nodes located in the armpits. Metastasis can confirm the enlargement of the lymph nodes, their soreness and compaction.
Diagnosis of breast cancer at an early stage: tests and examinations
The disease can be detected in the early stages of formation. A blood test will help to get a general picture of the patient's condition. The formation of the inflammatory process is confirmed by changes in the quantitative composition of leukocytes, the level of ESR, the level of anemia is estimated by hemoglobin. In oncology, the indicators differ from the norm.
A high level of leukocytes confirms the presence of an inflammatory process. Low hemoglobin increases all fears. Deviation from the norm does not always indicate the presence of a malignant process, because such changes occur during other diseases. Confirm or refute assumptions will help. Their presence is 100% indicative of a malignant process.
Determination of the level of hemoglobin, leukocytes and ESR is carried out according to a general blood test. A specific type of analysis is aimed at identifying tumor markers. These are proteins and antigens that are produced by cancer cells.
After a standard instrumental and differential study, a general and biochemical blood test is used. The data obtained as a result of the study of the material is quite enough to make an accurate diagnosis.
In addition to the standard procedure, a specialist can offer spectral analysis. This is a relatively recent development, during which it is possible to obtain the most reliable result. The technique is based on infrared spectra actively absorbing blood serum. This is a safe and informative type of diagnosis.
Diagnosis of breast cancer often supplemented by genetic analysis. This is a good way to identify hereditary predisposition to cancer. The choice of the optimal diagnostic technique is carried out by an experienced oncologist.